Heat Safety: Tips for Preparing for Summer Sports in Hot Weather
Blogs

Summer is here, which means many students are moving outdoors to participate in strenuous physical activities. Strenuous activities in hot environments place students at-risk for heat illnesses, including heat stroke.
In 2001, professional football player Korey Stringer died during practice from heat stroke. Though his death shined a light on heat illnesses, the deaths of young athletes continue.
Two decades after Stringer’s death, University of Cumberland wrestler Grant Brace died from heat stroke during wrestling practice. As reported by ESPN, his death was preventable. Though Brace begged for water and showed clear signs of heat exhaustion, he was denied water and even threatened by his coach to be kicked-off the wrestling team should he not continue in a team workout. The activity, according to USA Today, was sprinting up “Punishment Hill” on the first day of practice.
Alone, he collapsed as he searched for water.
There is no rationale to support the foolhardy belief that an athlete “pushing” themselves to the point of and beyond unsafe levels of thirst and heat make a tougher, or “better” athlete. In fact, all the evidence shows this to be an irresponsible, misguided, and potentially deadly mindset.
Regardless of heat safety training for staff and enhanced awareness on the dangers of heat illnesses, coaches continue to be implicated in the deaths of young athletes from heat stroke.
Exertional Heatstroke in High School Athletics
Exertional heat stroke (EHS) is an acute medical emergency caused by an excessive rise in body temperature, usually from physical exertion in high temperatures. EHS can occur when one’s body temperature rises to 104 F (40 C) or higher. In heatstroke, the body cannot regulate its own temperature.
Each year, EHS results in thousands of emergency room visits and hospitalizations throughout the nation. It is the leading cause of preventable death in high school athletics. Students participating in high-intensity, long-duration or repeated same-day sports practices and training activities in hot weather are at greatest risk.
The National Center for Catastrophic Sport Injury Research (NCCSIR) reports that 28 high school football players died of EHS from 2008 through 2017. High school athletes in other sports are also at-risk. Female cross-country athletes are as likely to suffer from heat-related illnesses as athletes in any other high school sport.
The danger of heat illness extends beyond athletics to any student (and employee) engaging in strenuous activities. Consider, for example, a band member carrying a heavy instrument while marching for long periods of time on hot asphalt.
How to Create a Culture of Heat Safety in High School Athletics
Creating a culture of heat safety in school activities and athletic programs can significantly reduce the risk of heat-related illnesses and keep your student-athletes performing at their best. Here are some essential steps to establish a culture of heat safety.
Three Ways to Create a Culture of Heat Safety in High School Athletics
1. Heat Safety Training for Staff and Coaches: Equip coaches and staff with the knowledge and skills to recognize and respond to heat-related illnesses promptly. Provide training on heat safety, including identification of symptoms, appropriate response measures, and emergency procedures. Encourage coaches and staff to stay vigilant and prioritize the well-being of student-athletes.
2. Creating a Heat Illness Prevention Plan: Create a clear and comprehensive heat illness prevention plan or policy that outlines guidelines for practice and competition in high-temperature conditions. These policies could include provisions for modifying or canceling practices and games based on heat levels, providing adequate hydration breaks, implementing appropriate uniform and equipment guidelines to enhance heat dissipation, and an emergency action plan for how to respond to heat illness.
3. Reinforcing Policies and Procedures: Consistently reinforce heat safety policies through ongoing communication and monitoring compliance. Encourage reporting of symptoms and concerns and establish a confidential reporting mechanism. Recognize and reward individuals and teams that prioritize heat safety. These efforts create a culture of accountability, ensuring the well-being of student-athletes.
Automate Your Heat Safety Training
Ensure all your staff and coaches regularly complete and pass all mandated and recommended heat safety training requirements with our managed training solution. They’ll automatically be enrolled in courses like Heat‐Illness Prevention for School Athletics (NFHS) and Heat‐Illness Prevention for Student Activities.
Components of Heat Illness Prevention in Student Activities
Training, heat prevention plans, and policies and procedures should address heat acclimation in sports, hydration, monitoring and adapting to environmental conditions, and emergency response plans.
1. Heat Acclimatization for Heat-related illness prevention for athletes
Heat illness is most common during the first 5 days of practice. In these first few days, activity supervisors should avoid making students do too much, too soon, while wearing too much gear.
Heat acclimatization helps to ready one’s body to cope with heat exposure. A 14-day heat acclimation period is vital to helping the body cope with heat stress while engaging in activities in hot environments.
The following chart summarizes the structure of a heat acclimation program:
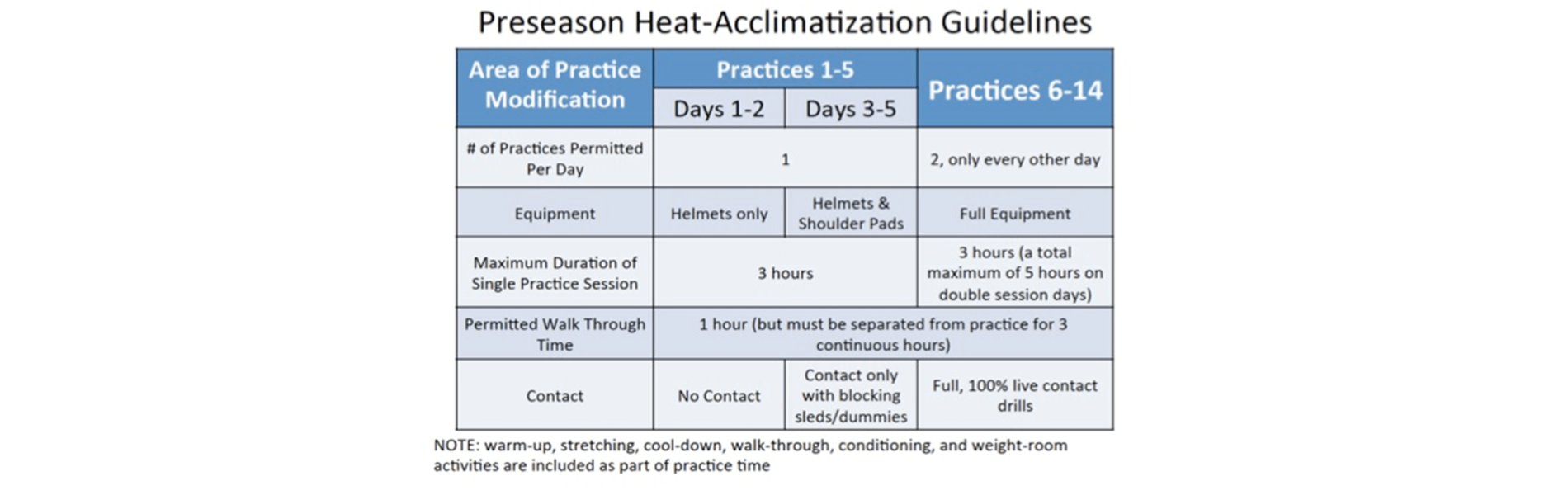
Many statewide school athletic associations have heat acclimatization in sports policies. The Korey Stringer Institute has compiled and evaluated each state’s policy. You can use this information to preview the components of your state plan.
Because the risk of exertional heat illnesses during the preseason heat-acclimatization period is high, the National Association Athletic Trainers’ Association strongly recommends an athletic trainer be on site before, during, and after all practices.
2. Hydration for Heat Illness Prevention
Dehydration occurs when the body loses fluids faster than they are taken in, depriving one’s body of the fluids it needs to carry out its normal functions.
By the time a person realizes they’re thirsty they are already moderately dehydrated, which makes focusing on adequate hydration outside of activities as important as hydrating during an activity.
Three Steps for Adequate Hydration:
- Pre-hydrate. Students should properly hydrate before engaging in physical activity.
- Stay hydrated. Students should replenish fluids during an activity to maintain a healthy level of hydration.
- Re-hydrate. The fluids lost during an activity must be replaced following the activity.
Water is the least expensive and most accessible fluid during exercise, though sports drinks help to replace lost salts and electrolytes and are recommended for use during intense exercise that is greater than 60 minutes or during intense exercise in the heat.
3. Monitoring and Adapting to Environmental Conditions to Prevent Heat Illness
An important step in heat illness prevention is adjusting the length and intensity of student activities to the environmental conditions. It’s important that school leaders, athletic directors, coaches, and athletic trainers monitor heat conditions and be prepared to shorten or cancel practice or games if temperatures reach dangerous levels.
What Temperature is Too Hot for Students to Practice or Play Sports?
The Wet Bulb Globe Temperature (WBGT) is an indicator of heat related stress on the human body in the direct sunlight. The American College of Sports Medicine (ACSM) has developed a set of values that have been accepted as a standard to follow. Guidelines were developed for both continuous and intermittent (non-continuous) activities.
This chart is for continuous activities with little if any breaks, such as cross-country running, 5K runs and marathons.

This chart is for intermittent activities that generally have breaks between bursts of high intensity actions, such as football, soccer, lacrosse, etc.

You can find WBGT forecasts on the National Weather Service’s National Digital Forecast Database page.
4. How to Treat EHS
If a student shows any symptoms of EHS, immediate action is needed to maximize their chance of survival.
EMS (9-1-1) should be called immediately.
Aggressive cooling of the entire body should be done as fast as possible to lower their body temperature. Whole-body cold-water immersion is the fastest way to cool the body. If this is not possible, the second option is to continually douse the individual’s body with water (e.g., a cold shower, running a hose over the entire body while covering the body with iced towels, etc.) while awaiting EMS.
Prioritizing heat safety in summer sports is crucial for the well-being and performance of student athletes. By understanding the risks of exertional heatstroke, establishing a culture of heat safety, and implementing key components of heat illness prevention, districts can create a safer environment for their students. Remember to educate coaches, staff, and athletes on the signs of heat illness, provide adequate hydration, modify activities in extreme heat, and regularly assess conditions. With proactive measures and a collaborative approach, districts can ensure that student athletes can enjoy their sports while minimizing the risk of heat-related injuries. By investing in heat safety, districts demonstrate their commitment to the health and well-being of their students, setting them up for success both on and off the field. Together, let’s make summer sports safe, enjoyable, and memorable experiences for all.
The National Federation for High School Athletics offers resources to learn more about heat illness prevention and hydration:
